Preimplantation Genetic Testing
Introduction:
Preimplantation Genetic Testing for Aneuploidy (PGT-A): Enhancing IVF Success
In the realm of assisted reproductive technology, Preimplantation Genetic Testing for Aneuploidy (PGT-A), formerly known as Preimplantation Genetic Screening (PGS), has emerged as a ground-breaking tool. PGT-A is utilized during in vitro fertilization (IVF) to assess the genetic health of embryos, enhancing the chances of a successful pregnancy. This blog will delve into the conditions PGT-A can detect, its various types, and the treatment process.
Conditions Detected by PGT-A
PGT-A primarily screens for aneuploidy, a condition characterized by an abnormal number of chromosomes in an embryo. Aneuploidy can lead to miscarriages or the birth of a child with genetic disorders like Down syndrome. By identifying aneuploid embryos, PGT-A improves the selection of the most viable ones, increasing the likelihood of a successful pregnancy.
Types of PGT-A
- Next-Generation Sequencing (NGS): This is the most advanced and widely used PGT-A technique. NGS allows for a comprehensive examination of all 24 chromosomes in a human embryo, providing detailed insights into their genetic health.
- Comparative Genomic Hybridization (CGH): CGH, which is now less common, analyses the entire genome of the embryo. It is a predecessor of NGS and is used in fewer IVF clinics today.
- Fluorescent In Situ Hybridization (FISH): FISH is an older, less precise technique that can only analyze a limited number of chromosomes. It has been largely replaced by NGS and CGH.
Conditions Detected by PGT-A
PGT-A primarily screens for aneuploidy, a condition characterized by an abnormal number of chromosomes in an embryo. Aneuploidy can lead to miscarriages or the birth of a child with genetic disorders like Down syndrome. By identifying aneuploid embryos, PGT-A improves the selection of the most viable ones, increasing the likelihood of a successful pregnancy.
The PGT-A Treatment Process
- Ovarian Stimulation: The IVF cycle begins with ovarian stimulation, where medications are administered to stimulate the ovaries to produce multiple eggs.
- Egg Retrieval: When the eggs are mature, they are retrieved using a minor surgical procedure.
- Fertilization: The eggs are fertilized with sperm in a laboratory dish to create embryos.
- Blastocyst Cultivation: Embryos are cultured for 5-7 days until they reach the blastocyst stage, at which point they can be biopsied.
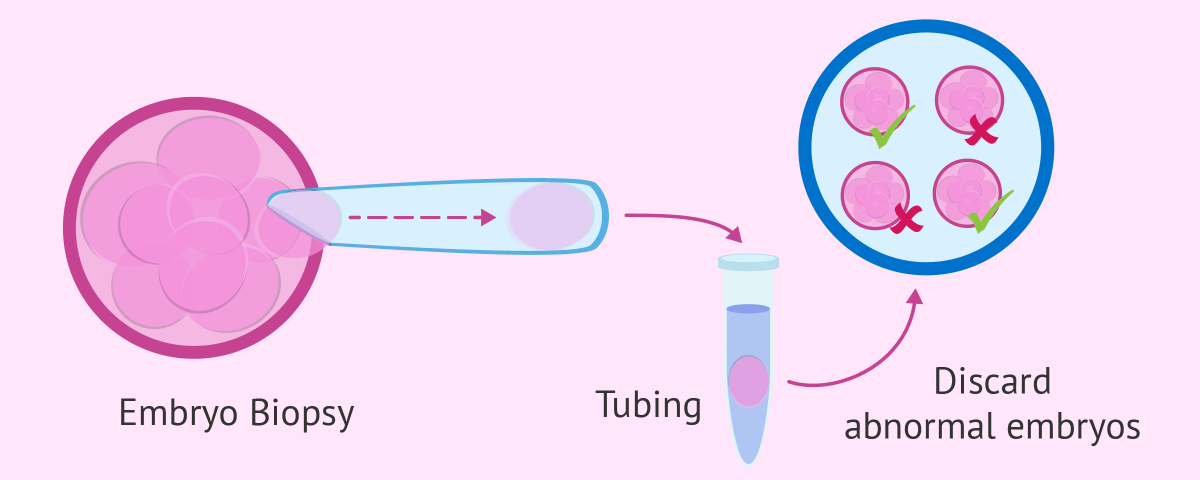
- Biopsy: A few cells are extracted from each blastocyst for genetic analysis.
- Genetic Testing: Using NGS, CGH, or other PGT-A techniques, the extracted cells are analyzed for chromosomal abnormalities.
- Embryo Selection: Embryos with a normal chromosomal profile are selected for transfer into the uterus.
- Embryo Transfer: One or more healthy embryos are transferred into the uterus, and the remaining embryos can be cryopreserved for future use.
- Pregnancy Test: A pregnancy test is performed approximately two weeks after the embryo transfer.
Conditions for PGT-A Utilization
PGT-A is recommended in several cases:
- Advanced maternal age: Women over 35 have an increased risk of aneuploidy.
- Repeated miscarriages or implantation failures.
- Severe male factor infertility.
- Prior chromosomal abnormalities in a previous pregnancy or child.
- Family history of genetic disorders.
Conclusion:
PGT-A is a remarkable advancement in assisted reproductive technology. It empowers couples struggling with infertility to select healthy embryos, significantly improving the success rates of IVF. By identifying aneuploid embryos, PGT-A reduces the risk of miscarriages and the birth of children with genetic disorders. Although it’s not a guarantee of pregnancy, it offers valuable information to make informed decisions on embryo selection and family planning. Couples considering IVF should consult with a fertility specialist to determine if PGT-A is the right option for them.

